After almost 150 years, we may at long last see how broad anesthesia makes us float into obviousness — albeit a portion of the points of interest stay dim.
These medications oust atoms held in the fatty membrane that encompasses brain cells. When the medications arrive at this greasy shell, the liberated particles bob around like billiard balls inside the film and modify the capacity of proteins installed in its surface, as per another examination in refined cells and natural product flies.
The new discoveries could help settle a riddle that has waited for quite a long time.
“People have been seriously hammering on this for at least 100 years,” said study creator Scott Hansen, a partner educator in the divisions of atomic medication and neuroscience at The Scripps Research Institute in La Jolla, California.
In any case, not every person figures the new examination can uncover why sedatives put people “to rest.”
“Let’s just say there’s a large difference between the fruit fly brain and the human brain,” said Dr. Emery Brown, a teacher of Medical Engineering and Computational Neuroscience at the Massachusetts Institute of Technology and an educator of Anesthesia at Harvard Medical School, who was not engaged with the examination.
Wellspring of unconsciousness
Since dental specialist Dr. William Morton previously utilized the concoction ether as a sedative during the 1840s, researchers have tried to see how the medication and different sedatives communicate with the mind. Nineteenth-century researchers speculated that sedatives by one way or another upset the greasy layer encompassing cells, including synapses, as the medications repulse water while promptly blending in with oils and fats, he said.
Later exploration, led during the 1980s, proposed that sedatives tie legitimately to proteins stopped inside the greasy layer and straightforwardly meddle with the movement of said proteins, driving down the general action of synapses, The Scientist revealed. In any case, Hansen and his partners presumed this wasn’t the entire story.
In tests in refined cells and organic product flies, the creators found that sedatives disturb explicit pockets of fat inside the cell film; those interruptions at that point free atoms and trigger chain responses somewhere else on the cell surface. The creators set that these sub-atomic changes, among different instruments, caused organic product flies to lose awareness, as confirm by the creepy crawlies getting stationary for a few minutes.
In any case, specialists disclosed to Live Science that these creature investigations can indeed reveal to us a limited amount of much about how the medications work in people.
While the investigation reconfirms that sedatives are “grimy medications,” which means they focus on various cell frameworks without a moment’s delay, it can’t state precisely how interruptions to the greasy film adjust cognizance, or even how those progressions change movement all through the mind, Brown disclosed to Live Science.
The medications upset the film, “okay, but now finish the story,” he said. “How does that then drive [activity in] certain parts of the brain?” Understanding how sedatives work could assist specialists with utilizing the medications all the more decisively in the facility, Brown said.
This comprehension may likewise indicate how the cerebrum normally moves all through cognizance, as it does during rest, Hansen included.
Propelled magnifying lens offer a more intensive look
“Back in the day,” when sedatives previously entered boundless use, researchers guessed that a large number of the physiological impacts of medications originated from changes to the greasy layer of cells, a door that decides when atoms may enter or exit, said Francisco Flores, an exploration researcher and teacher in the Anesthesia Department at Massachusetts General Hospital who was not associated with the investigation. As innovation advanced, researchers found that numerous medications interface with explicit proteins tied down in the fatty membrane, and along these lines, research endeavors concentrated more on these layer bound proteins than the fats encompassing them, known as lipids, he said.
“However, for anesthetics, the lipid hypothesis survived for longer,” Flores said. Sedatives can cross the blood-cerebrum obstruction, a fringe of cells that isolates flowing blood from mind tissue and permits just certain atoms to go through. All sedatives, just as different medications that pass the blood-cerebrum hindrance, repulse water and promptly communicate with lipids, “so there’s still a chance that they can do something in the membrane,” he said.
In any case, nineteenth-century researchers couldn’t see how anestheticsdistorted the lipid layer; the errand required super‐resolution magnifying lens that had not been concocted at that point, Hansen said. Hansen and his co-creators utilized such a microscope, called dSTORM, to see how cells responded when washed in the sedatives chloroform and isoflurane.
They found that various kinds of fats inside the cell layer responded diversely to the medications.
One pocket of fats, known as GM1, contains high centralizations of cholesterol particles, firmly stuffed together and specked with explicit sugar atoms. Upon presentation to sedative, the fats inside these GM1 groups spread out, and in doing as such, discharge different proteins that were enmeshed with them. One such protein, called PLD2, breaks to an alternate heap of fats and starts a progression of compound responses.
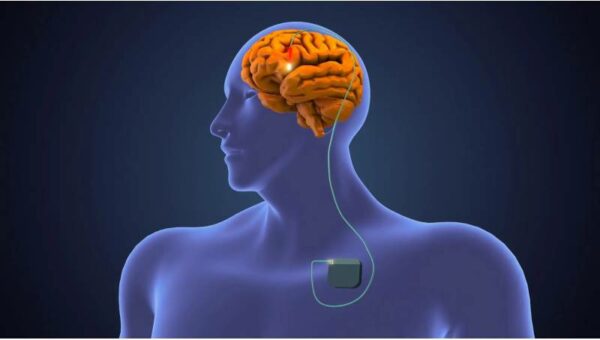
In particular, the response opens a passage through the phone called a TREK1 particle channel, which permits emphatically charged particles to leave the phone. In a synapse, this mass migration of positive particles makes the cell all the more adversely charged and could smother that cell’s electrical and synthetic movement. That, hypothetically, could drive the mind into an oblivious state, Hansen said.
In any case, it may not be that clear, Brown noted.
Still more riddles to unravel
To check whether their cell tests continued to creatures, the writers analyzed the cerebrums of organic product flies and found that, after introduction to chloroform, fats inside the lipid layers of the flies’ brain cells spread out similarly as had been seen in cell culture. Also, freak organic product flies without the capacity to make PLD2 got impervious to the chloroform treatment and required a bigger portion to become calmed, specialists announced in the investigation, which was distributed May 28 in the diary Proceedings of the National Academy of Sciences.
Since the freak flies were not totally immune to chloroform, the creators presumed that different components likely permit the medication’s sedative impact to grab hold. Disturbances to cells’ lipid film may add to this general impact, however now, their relative impact stays hazy, Brown noted. “Dirty” sedatives trigger various responses in the mind through various substance and metabolic pathways, and researchers don’t yet have a clue how film disturbances influence the general action inside that hardware, he said.
These cooperations will be hard to unravel in the to some degree basic fly cerebrum, and considerably all the more testing to comprehend in the human mind, Brown said.
All things considered, Hansen and his co-creators theorize that film disturbances may play a more extensive, overlooked job in the impacts of sedatives on people. Hypothetically, sedatives may by implication influence numerous proteins by first disturbing the lipid layer, Hansen said. Numerous proteins stopped in the lipid film have unsaturated fats adhered to their structures, for example, and a portion of these proteins cooperate with cerebrum synthetic concoctions and help drive action of synapses. One theory is that if sedatives focus on the unsaturated fats appended to these proteins, the medications could possibly adjust their capacity and steady the cerebrum, Hansen said.
“Again, this is speculative,” and would should be affirmed with future studies, he included. Comparable examinations ought to be finished with different medications that cross the blood-cerebrum hindrance, not only anesthetics, to decide if the impact seems extraordinary or normal to numerous classes of medication, Flores said. Hansen said he needs to see whether synthetic compounds with comparative impacts as of now exist in the cerebrum, and maybe help put us to sleep.
While the new investigation opens many intriguing roads for future exploration, for the present, the outcomes remain genuinely starter, Brown said.
“Do I do something different in the operating room now that I’ve read that paper? No,” Brown said.